Navigation links
- Introduction
- Skin: epidermal layers
- Skin: dermal layers
- Sudoriferous (sweat) and sebaceous (oil) glands
- Hair and nails
- Skin color
This most extensive organ system has the skin and accessory structures, including hair, nails, glands (sweat and sebaceous), and specialized nerve receptors for stimuli (changes in internal or external environment) such as touch, cold, heat, pain, and pressure. Its functions include protection of internal structures, prevention of entry of disease-causing microorganisms, temperature regulation, excretion through perspiration, pigmentary protection against ultraviolet sunrays, and production of vitamin D. The body stores about half its fat in the underlying hypodermis.
The skin is the largest organ of the body, with a surface area of 18 square feet. Its two main layers are the epidermis (outer layer) and dermis (inner layer). The epidermis has several strata (layers) that contain four cell types. Keratinocytes produce keratin, a protein that gives skin its strength and flexibility and waterproofs the skin surface. Melanocytes produce melanin, the dark pigment that gives skin its color. Merkel's cells are probably involved with touch reception. Langerhans' cells help the immune system by processing antigens (foreign bodies).
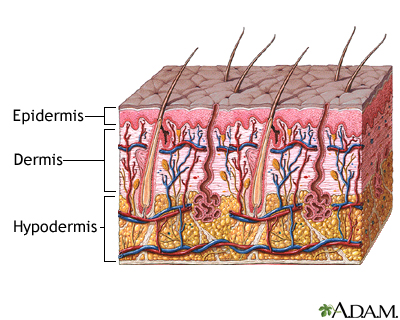
The deepest layer of the epidermis, the stratum basale, is a single layer of cells resting on a basement membrane (layer between the dermis and epidermis). The stratum basale cells divide continuously. As new cells form, older ones are pushed toward the skin surface.
The epidermis does not have a direct blood supply; all nutrients that feed these cells come from the dermis. Only the deepest cells of the stratum basale receive nourishment. The cells that are pushed away from this layer die. When the cells reach the skin surface, they are sloughed off in a process called desquamation.
The next layer, the stratum spinosum, consists of spiny prickle cells that interlock to support the skin. The stratum granulosum, the thin middle layer, initiates keratinization (production of keratin). This process starts the death of epithelial cells (the cell type that makes up skin).
During desquamation, keratinocytes are pushed toward the surface. These cells begin to produce the keratin that eventually will dominate their contents. When these cells reach the epidermis outer layer, they are little more than keratin-filled sacs. Millions of these dead cells are worn off daily, creating a new epidermis every 35 to 45 days.
The stratum lucidum protects against sun ultraviolet-ray damage. This thick layer appears only in frequently used areas such as palms of the hands and soles of the feet. Thick skin epidermis has all five strata. Thin skin covers thinner epidermal areas such as eyelids. Thin skin has three or four of the five strata; it never has stratum lucidum.
The stratum corneum, the fifth, outermost layer is thick with rows of dead cells. These cells contain soft keratin, which keeps the skin elastic and protects underlying cells from drying out.
The dermis, called "true skin, " is the layer beneath the epidermis. Its major parts are collagen (a protein that adds strength), reticular fibers (thin protein fibers that add support), and elastic fibers (a protein that adds flexibility). The dermis has two layers: the papillary layer, which has loose connective tissue, and the reticular layer, which has dense connective tissue. These layers are so closely associated that they are difficult to differentiate.
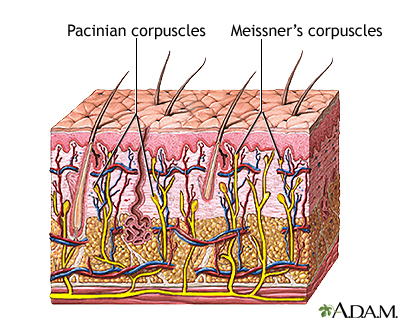
The papillary layer lies directly beneath the epidermis and connects to it via papillae (finger-like projections). Some papillae contain capillaries that nourish the epidermis; others contain Meissner's corpuscles, sensory touch receptors. A double row of papillae in finger pads produces the ridged fingerprints on fingertips. Similar patterns in the ridged fingerprints on fingertips are on palms of the hands and soles of the feet. Fingerprints and footprints keep skin from tearing and aid in gripping objects.
The reticular layer of the dermis contains criss-crossing collagen fibers that form a strong elastic network. This network forms a pattern called cleavage (Langer's) lines. Surgical incisions that are made parallel to cleavage lines heal faster and with less scarring than those made perpendicular. Parallel incisions disrupt collagen fibers less and require less scar tissue (cells that aid in healing) to close up a wound.
The reticular layer also contains Pacinian corpuscles, sensory receptors for deep pressure. This layer contains sweat glands, lymph vessels, smooth muscle, and hair follicles, described in the discussion on hair follicles later in this overview.
The hypodermis (subcutaneous layer) lies beneath the dermis. Loose connective tissue such as adipose tissue (fat) insulates the body, conserving heat. It also contains blood vessels, lymph vessels, and the bases of hair follicles and sweat glands. The fat distribution in this layer gives the female form its characteristic curves.
Sudoriferous (sweat) and sebaceous (oil) glands
Skin produces associated structures such as sudoriferous (sweat) glands and sebaceous (oil) glands. It also produces fingernails, hair, and sensory receptors that enable humans to feel pressure, temperature, and pain.
Both groups of sudoriferous glands (sweat glands) are in most of the body: eccrine glands are coiled ducts deep in the skin that connect to the surface; apocrine glands are in armpits, areolae of nipples, and the genital region. Eccrine glands secrete sweat, a mixture of 99 percent water and 1 percent salts and fats. In warm conditions with low humidity, perspiration (secretion of sweat) and evaporation cool the body.
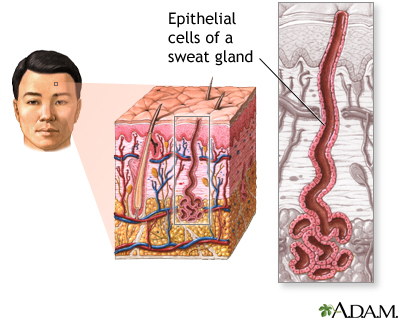
Apocrine glands, which become active at puberty, are larger, deeper, and produce thicker secretions than eccrine glands. The apocrine glands secretions contain pheromones, substances that enable olfactory (sense of smell) communication with other members of the species. This communication provokes certain behavioral responses such as sexual arousal. Unlike eccrine glands that respond to heat, apocrine glands respond to stress and sexual activity by secreting sweat with a characteristic odor. This odor differs from body odor that results from bacteria decomposing skin secretions on the skin.
Ceruminous glands are modified apocrine glands in the external ear canal lining. They secrete cerumen (earwax), a sticky substance that is thought to repel foreign material.
Mammary glands in female breasts are modified apocrine glands. These glands are adapted to secrete milk instead of sweat.
Sebaceous glands (oil glands) are all over the body except on the palms of hands and soles of feet. The glands empty via ducts into the bases of hair follicles and secrete sebum (a mixture of fats, waxes, and hydrocarbons). Sebum keeps hair moist and prevents skin from drying. Sebaceous glands are numerous on the face and scalp. During puberty, increased sex hormone levels in the blood may produce excessive sebum. This over secretion plugs the gland and hair follicle, producing a skin disorder called acne.
Hair is composed of cornified threads of cells that develop from the epidermis and cover most of the body. Each hair has a medulla, cortex, and cuticle. The medulla in the center contains soft keratin and air. The cortex, the innermost thickest layer, has the pigment that gives hair color. The cuticle, the outermost layer, has cells that overlap like scales. Both the cuticle and cortex have hard keratin.
The hair root in a hair follicle is embedded beneath the skin. The hair shaft protrudes from the skin. Hair sheds and is replaced constantly during growth and rest phases. Hair has a protective function: eyebrows keep sweat from running into the eyes, nose and ear hairs filter dust from the air, and scalp hairs protect against abrasion and overexposure to sun rays.
Hair follicles extend into the dermis; the deep ends expanded parts are called hair bulbs. A papilla (connective tissue protrusion that contains capillaries) protrudes into the hair bulb and provides nutrients for the growing hair. The hair follicle walls have an inner epithelial root sheath and an outer dermal root sheath. The epithelial root sheath has an inner and an outer layer that thins as it approaches the hair bulb. It becomes the matrix, the actively growing part of the hair bulb that produces the hair.
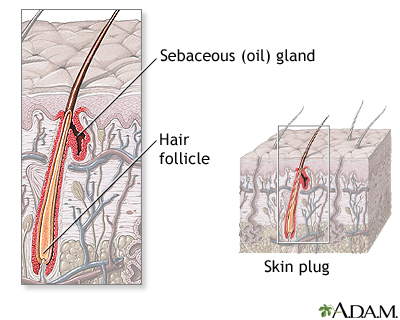
Arrector pili muscles are smooth muscle cells attached to hair follicles. When they contract, they pull the hair into an upright position, causing skin dimples (goose bumps). The nervous system regulates these muscles; cold temperatures or fright can activate them.
Hair development begins in the third fetal month. By the fifth month, lanugo (thin hair) covers the fetus. At 5 months, lanugo disappears from every area except the scalp and eyebrows where coarser hair replaces it. Vellus (a film of delicate hair) eventually covers the rest of the body. Terminal hair is the early coarse scalp and eyebrow hair and later armpit and genital hair that grow during puberty. No new hair follicles develop after birth.
Like hair, nails develop from the epidermis. These hard plates of keratinized cells are at the ends of fingers and toes. Nails appear pink because their translucency reveals the vascular tissue beneath. They aid in grasping objects, scratching, and protecting fingers and toes.
The components of the nail are the lunula, body, root, and free edge. The lunula is the white half-moon shaped part at the nail base. Both the body and free edge region that overhangs the end of the finger or toe are visible. The nail rests on the thick layer of epithelial skin called the nail bed. The root is hidden under skin folds. Under the root lies the matrix (thick layer of skin). Eponychium (thin layer of epithelium) covers the nail during development; in the adult, it remains at the nail base only and is called the cuticle. The hyponychium is the epithelium of the nail bed.
Skin color results from the presence of melanin, carotene (yellow to orange pigment), and underlying blood reflected through skin. Melanin keeps excessive ultraviolet rays from burning the skin. Exposure to sunlight causes the skin to produce more melanin, causing suntan, a temporary change in skin color. Melanin-rich cells continually move toward the surface, where they are sloughed. Too much sun is dangerous to skin; it increases the risk of cancer by affecting the genetic material of cells.
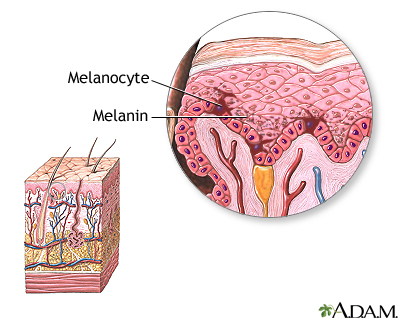
Variety of skin color is caused mainly by the number and distribution of melanocytes. Darker skin has more melanin that is produced by more melanocytes. However, the different skin colors among individuals and races do not reflect different numbers of melanocytes; instead, they show different kinds and amounts of melanin production by melanocytes. Oriental skin has a greater amount of carotene in the stratum corneum, producing a yellowish tinge. Albinism is a condition where skin does not produce melanin.
The information provided herein should not be used during any medical emergency or for the diagnosis or treatment of any medical condition. A licensed medical professional should be consulted for diagnosis and treatment of any and all medical conditions. Call 911 for all medical emergencies. Links to other sites are provided for information only -- they do not constitute endorsements of those other sites. © 2001 - A.D.A.M., Inc. Any duplication or distribution of the information contained herein is strictly prohibited.